Make an Appoinment
Non-surgical and minimally invasive procedures to find and treat structural or electrical problems in the heart.
About
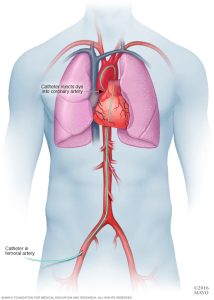
A coronary angiography procedure involves viewing the blood vessels in your heart with an X-ray. The test is typically performed to determine whether there is a reduction in the blood flow to the heart. They are a part of a larger group of procedures referred to as a heart (or cardiac) catheterization.
Need
A coronary angiography can help identify the blood vessel obstructions and demonstrate its level of obstruction. It will also spot Atherosclerosis aka show how many of your coronary arteries are obstructed or constrained by fatty plaques. Furthermore, it will verify the outcome of any prior coronary bypass operation and the heart’s and your blood vessels’ blood flow.
Angiograms typically follow non-invasive heart tests like an electrocardiogram, an echocardiography, or a stress test.
Process
An angiography typically lasts an hour, but this time might vary, especially if additional cardiac catheterization procedures are performed at the same time.
An X-ray machine- visible dye is injected into your heart’s blood arteries during a coronary angiography. Your blood vessels become visible on the X-ray equipment through a sequence of images called angiograms. During coronary angiography, your doctor may perform angioplasty, or the opening of blocked heart arteries.
About
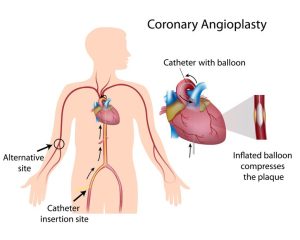
Coronary angioplasty, also known as percutaneous coronary intervention (PCI), is used to clear clogged coronary arteries brought on by coronary artery disease. . A tiny balloon catheter is placed during the procedure to assist widen a blood artery that has become narrowed and enhance blood flow to the heart.
Without requiring open heart surgery, it restores blood flow to the heart muscle. An emergency situation, such as a heart attack, may call for an angioplasty. Alternatively, if your doctor has a strong suspicion that you have heart problems, the procedure might be performed as an elective.
Need
A blood clot may form on the surface of the coronary arteries when the plaque built up ruptures. Blood supply to a region of the heart muscle may be partially or entirely blocked if the clot grows large enough. Opening a blockage as soon as possible restores blood flow to the heart muscle and decreases the damage that a heart attack does to the heart. The best course of action during a heart attack is an angioplasty, which can open the artery immediately.
Opposed to CABG, angioplasty has the drawback of potentially causing the artery to narrow again in the future. When stents are utilised, especially those that are drug-coated, the likelihood of this occurring is reduced.
Process
After an angiogram, ready with the images of any blockages and their locations, the doctor proceeds with the angioplasty.
Your doctor will inflate the balloon in the blockage to force the plaque against the artery wall. This increases arterial opening and enhances blood flow.
The freshly opened portion is typically fitted with a small mesh tube known as a stent. Stents support the artery and reduce the likelihood of re-narrowing. Stents resemble tiny springs and are comprised of metal mesh.
Drug-eluting stents are stents that have a coating of medication that releases drugs into the artery gradually and constantly. These medications aid in preventing scar tissue that forms around the stent from obstructing the artery again.
Occasionally, angioplasty involves the removal of plaque. A catheter with a rotary shaver on its tip is introduced into the artery during a treatment known as an atherectomy to remove plaque. Additionally, the plaque is broken apart or disintegrated using lasers. Due to angioplasty’s superior outcomes for the majority of patients, these operations are now rarely performed.
About
Patients with significant calcification in their coronary arteries (hardened arteries) undergo the sophisticated and difficult procedure known as rotational atherectomy (rotablation). It basically involves drilling with a specific diamond tip burr that rotates between 150,000 and 200,000 times per minute. This drilling procedure cleans the interior of the arteries to facilitate the balloon and stent’s easy passage. This approach makes use of larger tubes or catheters than a normal one. Only Interventional Cardiologists with extensive training employ this method, and only in specific circumstances.
Need
Patients with angina pectoris can benefit from this surgery for the treatment of coronary heart disease. Plague, a fatty substance consisting of cholesterol, calcium, and other substances, tends to accumulate in the arteries over time. This causes either a partial or complete blockage of that artery, which can result in a heart attack, stroke, or painful blood vessel obstructions in the legs. If the plaque is soft enough, an angioplasty is enough to remove the plaque to revive the artery and restore the blood flow. Conversely, rotating atherectomy( rotablation), is used when the plaque is too stubborn to be removed by angioplasty.
Process
Long-term calcium buildup in the artery walls can result in the plaque becoming incredibly rigid and hard, to the point where an angioplasty balloon cannot enlarge the artery. Here comes in the rotablator, a tiny gadget, to solve this issue. It also goes by the name “diamond rotor” since one of its ends has a burr covered in diamond dust. After the drill head has been inserted into the affected artery, balloon angioplasty is used to expand the region. For the stents to fully expand, high pressure balloons are frequently used. The placement of the drug-eluting stent follows. These stents gradually release a medication to prevent recurrent arterial blockage. This guarantees long-term treatment efficacy.The rotablator drills into the hardened plaque, simultaneously shredding it into tiny fragments. These tiny fragments can then be eliminated by the body, once safely ingested into the bloodstream.
About
In comparison to non-calcific plaques, a large number of lesions treated with transcatheter interventions in the coronary and peripheral vascular beds have moderate to severe calcific plaques, which are known to indicate inferior procedural success rates, an increase in peri-procedural adverse events, and negative clinical outcomes. Intravascular lithotripsy (IVL), a revolutionary method for treating highly calcific plaque lesions, uses acoustic shockwaves in a balloon-based delivery system and is adapted from lithotripsy technology used to treat ureterorenal calculi. Calcium fractures triggered by the shockwaves make it easier for stent expansion and luminal gain.
Process
Shockwave Intravascular Lithotripsy uses Sonic Pressure Waves (Sound waves) to crack the calcium in the coronary artery.A small balloon is inflated at the site of the calcium & Shockwave’s are emitted through special lithotripsy emitters integrated within the balloon. These sonic waves travels through the coronary tissues & fracture the calcium present in the blockage. Stent expansion is easily done after an IVL treatment.IVL is one of the latest technology available for treating calcified blockages. The therapy offers high level of safety & efficacy. It consists of a generator & a catheter which has an array of emitters that emits high frequency sound waves to the target blockage.
Intravascular ultrasound, or IVUS produces images of the interior of blood arteries using sound waves produced by a transducer or probe. IVUS uses an innovative catheter with a tiny ultrasonic transducer on one end. The catheter is guided to the desired spot through an artery or vein. T he transducer then produces sound waves to create images of the blood vessels and aid in the examination of various problems.
It is also known as Endovascular ultrasonography or intravascular echocardiography.IVUS can display the complete arterial wall and offer crucial details on the amount and kind of plaque buildup, which can assist in predicting your risk of having a heart attack. In addition to not using ionising radiation and having no known negative effects, ultrasound also generates detailed images of soft tissues that are difficult to see on x-rays.There is little to no prior preparation needed for this process. However, medical professionals frequently combine it with another therapy.
Process
On top of a skinny tube called catheter is a tiny ultrasound wand. The catheter is placed into a groin artery and advanced toward the heart. It differs when compared to traditional duplex ultrasonography. The ultrasound transducer is placed on the skin to perform duplex ultrasound from outside of the body.A computer converts the sound waves into images by analysing the way that blood vessels reflect the sound waves. IVUS allows a doctor to see inside your coronary arteries, giving them a more comprehensive view.
A procedure often includes IVUS. Some motives for doing so include:
- Obtaining knowledge about the heart’s blood vessels or determining whether cardiac surgery is necessary
- Addressing some cardiac diseases
A general view of the coronary arteries is provided via angiogram. It is unable to display the artery walls, though. IVUS scans can show cholesterol and fat deposits and disclose the arterial walls. Your chance of having a heart attack can escalate as these deposits accumulate.Professionals get a better understanding of stent restenosis or how the stents get clogged.
About
Fractional flow reserve(FFR) measures the ratio between the peak blood flow that can be achieved in a diseased coronary artery and the peak flow that might theoretically be achieved in a normal coronary artery. The range of a normal result is 0.94 to 1. Any value below that indicates that you require medical attention since your blood flow is not as high as it should be. For instance, if your FFR is 0.75, the narrow portion of your coronary artery is responsible for a 25% reduction in pressure. The widespread consensus is that myocardial ischemia is linked to an FFR of less than 0.75-0.80.
The FFR ratio between the coronary pressure distal to a coronary artery stenosis and the aortic pressure at maximal myocardial hyperemia can be determined by using a pressure wire during standard coronary angiography. The possible reduction in coronary flow distal to the coronary stenosis is represented by this ratio.
Process
This test can be necessary if your doctor determines that you need an angioplasty and a stent in one of your coronary arteries.
When imaging reveals you have a 50% to 70% diameter narrowing, providers employ this affordable, straightforward test. In some circumstances, healthcare professionals may examine the fractional flow reserve in patients with narrowing up to 90%.
If your narrowing is greater than 70% or less than 30%, you shouldn’t require this test. Based on the fact that it is obvious if you have minor stenosis, you do not require angioplasty, but if your number is large, you do.
About
A pacemaker is a little gadget that is implanted in the chest to assist in controlling the heartbeat. It keeps the heart from beating too slowly. A surgical procedure is necessary to implant a pacemaker in the chest. Depending on your situation, you may have one of the pacemakers listed below.
1)Single Chamber pacemaker: This kind often delivers electrical impulses to your heart’s right ventricle.
2) Double Chamber pacemaker: To help regulate the timing of contractions between the two chambers of your heart, this type sends electrical impulses to the right ventricle and right atrium.
Need
A pacemaker is implanted to assist in the control of your heartbeat. When you have a slow heartbeat (bradycardia) after a heart attack, surgery, or medication overdose but your heartbeat is otherwise expected to recover, your doctor may recommend a temporary pacemaker. A pacemaker can be permanently implanted to treat heart failure or to correct a chronic slow or irregular heartbeat.
Process
Pacemakers only function when they are required. The pacemaker sends electrical signals to your heart to adjust the beat if it beats too slowly (bradycardia).Sensors in some newer pacemakers detect body motion or breathing rate and signal the devices to increase heart rate during exercise as needed.
A pacemaker is made up of two parts:
1) Pulse generator: The electrical circuitry that regulates the frequency of electrical pulses delivered to the heart is housed in this tiny metal container along with a battery.
2) Leads (electrodes): One to three flexible, insulated wires are placed in one or more chambers of the heart to deliver electrical pulses that regulate the heart rate. Some newer pacemakers, however, do not require leads. These leadless pacemakers are surgically implanted directly into the heart muscle.
About
Cardiac resynchronization therapy is a procedure in which a device is implanted in the chest to cause the heart’s chambers to squeeze (contract) more organised and efficiently. Cardiac resynchronization therapy (CRT) employs a biventricular pacemaker, also known as a cardiac resynchronization device, to send electrical signals to both lower chambers of the heart (right and left ventricles). The signals cause the ventricles to contract in a more coordinated manner, which improves blood flow out of the heart.
In some cases, the device also includes an implantable cardioverter-defibrillator (ICD), which can shock the patient’s heart back to normal rhythm if it starts to beat dangerously irregularly.
Need
Patients with heart failure whose lower heart chambers (ventricles) don’t contract in unison can receive treatment with cardiac resynchronization therapy. It is widely used for patients with left bundle branch block, a condition that causes heart failure, as well as for those whose low heart rates make cardiac pacing likely to be necessary.
As a result of heart failure, your heart muscle may not be strong enough to pump out enough blood to sustain your body. If the chambers of your heart aren’t beating in unison, this could get worse. Cardiac resynchronization therapy may lessen heart failure symptoms and reduce the risk of fatal heart failure consequences.
Process
A minor surgical procedure is required to implant a device in the chest for cardiac resynchronization therapy. During surgery, insulated wires (leads, also known as electrodes) are inserted into a major vein under or near the collarbone and moved to the heart with the help of X-ray images. Each wire has one end attached to the appropriate position in the heart. The other end connects to a pulse generator, which is typically implanted beneath the skin beneath the collarbone.
Cardiac resynchronization therapy devices include:
- Cardiac resynchronization therapy with a pacemaker (CRT-P). The pacemaker is connected to the right upper chamber of the heart (right atria) and both lower chambers via three leads.
- Cardiac resynchronization therapy with a pacemaker and an ICD (CRT-D). For those with heart failure who also run the risk of sudden cardiac death, this device might be suggested. It can detect dangerous heart rhythms and deliver a more powerful energy shock than a pacemaker. This shock has the potential to reset the heartbeat.
About
A small, battery-operated device called an implantable cardioverter-defibrillator (ICD) is inserted into the chest to identify and treat irregular heartbeats (arrhythmias). An ICD continuously monitors the heartbeat and, if necessary, delivers electric shocks to restore a normal heart rhythm.
Need
If you have a dangerously fast heartbeat that prevents your heart from supplying enough blood to the rest of your body (such as ventricular tachycardia or ventricular fibrillation) or if you are at high risk of such a heart rhythm problem (arrhythmia), typically due to a weak heart muscle, your doctor may recommend an ICD. Other reasons why you might benefit from an ICD include:
- A history of coronary artery disease and a heart attack, both of which have weakened the heart
- An enlarged heart muscle.
- Long QT syndrome which is a genetic heart condition that increases the risk of dangerously fast heart rhythms
Process
A minor surgical procedure is required to implant a device in the chest.During surgery to implant the ICD, the doctor uses X-ray images to guide one or more flexible, insulated wires (leads) into veins near the collarbone to the heart. The leads’ ends connect to the heart. The other ends connect to a shock generator implanted beneath the skin beneath the collarbone. Once the ICD is in place,it will be tested and programmed as per your hearts rhythm needs. Depending on your heartbeat, an ICD could be programmed for:
Low-energy pacing : When your ICD responds to minor changes in your heartbeat, you may feel nothing or a painless fluttering in your chest.
A higher energy shock : The ICD may deliver a higher energy shock if the heart rhythm problem is severe. This shock can be excruciating, giving you the sensation of being kicked in the chest. The pain is usually brief, and there should be no discomfort after the shock is over.
About
Peripheral artery disease (also known as peripheral arterial disease) is a common condition characterised by narrowed arteries that restrict blood flow to the arms or legs. In peripheral artery disease (PAD), blood flow to the legs or arms — usually the legs — is insufficient to meet demand. This can result in leg pain when walking (claudication) as well as other symptoms. Peripheral artery disease is typically caused by the accumulation of fatty deposits in the arteries (atherosclerosis). Atherosclerosis causes artery narrowing, which reduces blood flow to the legs and, in some cases, the arms.
Need
Treatments for peripheral artery disease include lifestyle changes and sometimes, medication. In some cases, angioplasty or surgery may be necessary to treat peripheral artery disease that’s causing claudication.
Process
Peripheral Angioplasty & with Stent placement procedure is performed to clear clogged arteries. It is capable of both diagnosing and treating a blocked vessel. A thin, flexible tube (catheter) is guided to the narrowed section of the artery by the health care provider. To widen the blocked artery and improve blood flow, a tiny balloon is inflated. To keep the artery open, a small wire mesh tube (stent) may be placed.
About
An intra-aortic balloon pump (IABP) is a type of therapeutic device. It assists your heart in pumping more blood. The IABP is made up of a thin, flexible tube known as a catheter. A long balloon is attached to the catheter’s tip. This is referred to as an intra-aortic balloon, or IAB. The catheter’s other end connects to a computer console. This console has a mechanism that inflates and deflates the balloon when your heart beats.
Your heart circulates oxygenated blood and nutrients throughout your body. The blood vessels that carry oxygenated blood leave the heart via the arteries. Arteries can be found within the heart’s outer walls. These are known as coronary arteries. When the heart contracts, blood is pumped into the body. Blood flows into the coronary arteries as it relaxes, bringing oxygen to the heart. An IABP improves blood flow into your coronary arteries. With each contraction, it also helps your heart pump more blood.
Need
Cardiogenic shock is treated with IABP therapy. This occurs when your heart is unable to pump enough blood to meet your body’s needs.
Cardiogenic shock can be caused by a variety of heart problems. These include unstable angina, heart attack, certain abnormal heart rhythms, heart attack, heart failures. You may also require an IABP if you are undergoing a medical procedure. You might require it, for instance, if you undergo a percutaneous coronary intervention. This procedure opens a heart artery that has become blocked. An IABP may also be advantageous if you have heart surgery.
Process
The balloon-tipped catheter is inserted into a blood vessel and advanced to the heart during IABP therapy. This usually occurs during a heart surgery. A medical team may insert it at your bedside in an emergency.
A small incision will be made in the upper part of your inner thigh to access an artery. There will be an insertion of the balloon catheter. A surgeon will guide the catheter to a section of the aorta in your chest, monitoring the movement using continuous X-ray imaging. The balloon will be programmed to inflate when your heart relaxes and deflate when your heart contracts. The end of catheter will be secured.
About
An electrophysiological examination is a diagnostic procedure that examines the electrical activity of the heart and enables the physician to identify and evaluate rapid or irregular heartbeats. Compared to an external electrocardiogram (ECG), it can provide more comprehensive information. It involves a fine tube called a catheter being inserted into the heart via a blood vessel (vein or artery) in the groin. This catheter’s tip features a unique electrode that stimulates the heart and records electrical activity, enabling the doctor to pinpoint the source of any potential issues.
An aberrant cardiac rhythm can be managed or corrected using radiofrequency ablation. Similar to an electrophysiology study (EPS), it is carried out by introducing catheters into the heart through the groin. Then, the little region of the heart that is causing the aberrant electrical activity is destroyed using radiofrequency energy (heat). This can be carried out concurrently with the EPS or separately.
Need
The symptoms of palpitations or a racing heartbeat, which can be extremely upsetting at times for some people, would typically have been present. This is owing to the fact that the electrical conduction system in the heart can occasionally go in a different direction as a result of additional electrical connections known as “pathways” or more electrical cells. These pathways are frequently present at birth, although they may not produce symptoms until later in life. Ectopic beats (additional heartbeats) can move both up and down the normal conduction system when they occur in the heart. If this keeps happening, palpitations can occur. This describes when the heart suddenly starts to beat quickly and you become aware of it.
Process
The blood vessel in your groyne is then punctured with a sheath (similar to a cannula) and thin, flexible tubes (known as catheters) are inserted through it. Using an X-ray machine, the catheters are carefully guided into the right position inside your heart. As the catheters are placed, you can experience an odd feeling or discomfort in your chest, but this shouldn’t hurt.
Once the wires are in place inside the heart, an external pacemaker is used to deliver additional beats, which may cause your palpitations. This is required to identify the region of the heart that is causing the aberrant rhythm. It just takes a few seconds to restore the heart’s normal rhythm.
The surgeon will start to ablate the pathway or area of additional electrical cells if the problem has been identified and if it is deemed necessary. This is accomplished by transmitting radio frequency energy down the catheter cable to the desired location inside the heart.