Make an Appoinment
Surgical procedure that involves the heart, or the blood vessels that carry blood to and from the heart.
About
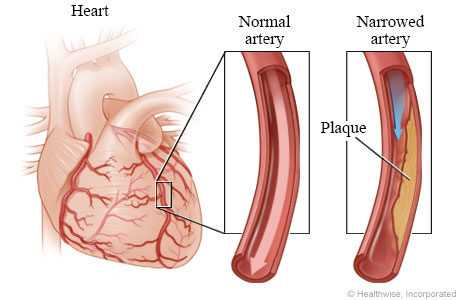
Coronary Artery Bypass Grafting (CABG), also known as Coronary bypass surgery, reroutes blood around a portion of a heart artery that is obstructed or partially clogged. A blockage in an artery can stop the flow of blood, which can result in heart attacks or heart attack-like symptoms. By rerouting blood vessels from other parts of your body around obstructions, CABG restores blood flow.
The cardiac condition that led to the blockages, such as atherosclerosis or coronary artery disease, is not treated by coronary bypass surgery. It can, however, reduce symptoms like shortness of breath and chest pain. This surgery can enhance heart health and lower the chance of dying from heart disease in some patients.
Need
You may need Bypass surgery if
- Your heart muscle suffers from acute chest discomfort brought on by the constriction of numerous arteries that supply it, depriving it of blood during even light activity or rest.
- Your left ventricle, the heart’s primary pumping chamber, isn’t working properly, and you have several damaged coronary arteries.
- The left major coronary artery is completely obstructed or significantly constricted. The left ventricle receives the majority of its blood from this artery.
- You have an arterial blockage that cannot be addressed using a technique that temporarily widens the artery by inserting and inflating a tiny balloon (angioplasty).
- A previous angioplasty or the implantation of a stent to keep the artery open failed. Or the artery has re-narrowed after a stent was implanted.
It may also be done in emergency situations like heart attack.
Process
The majority of coronary bypass procedures are performed while a heart-lung machine maintains blood and oxygen flow throughout your body through a lengthy chest incision. This is known as on-pump coronary bypass surgery.
The heart is made visible by the surgeon cutting down the middle of the chest at the breastbone and opening the rib cage. Following the opening of the chest, the heart is momentarily stopped by medicine, and the body’s blood circulation is handled by a heart-lung machine. In order to reroute blood flow around the sick artery’s restricted portion, the surgeon takes a length of healthy blood vessel, frequently from inside the chest wall or from the lower leg, and joins the ends above and below the blocked artery.
Other surgical techniques that your surgeon may employ are:
- Off-pump or beating-heart surgery : In order to stabilise the part of the heart the surgeon is operating on during this operation, surgery must be performed while the heart is beating. This is a challenging procedure as the heart is continuously beating during the operation.
- Minimally invasive surgery :Through tiny incisions in the chest, a surgeon performs coronary bypass surgery. Frequently using robotics and video imaging to aid the surgeon work in a limited space Port-access surgery or keyhole surgery are two variations of minimally invasive surgery.
Process Videos
Video 1 : CABG with Internal Mammary Artery
About
Coronary artery bypass grafting (CABG) that needs to be redone is more daunting than primary CABG in several ways. Re-CABG patients tend to be older, have more comorbid conditions, and have more sclerotic coronary and non-cardiac arteries than those who have primary CABG. Dissection of the heart is required, surgical treatments are more difficult, and entry of the sternum can occasionally be challenging. The patent left internal thoracic artery (ITA) anastomosed to the left anterior descending artery (LAD) must not be damaged if the patent vein grafts are unhealthy since they can be causes of thromboembolism. The frequent application of ITA to the LAD during first CABG, aggressive percutaneous coronary intervention (PCI) by interventional cardiologists, and best-practice medical management following primary CABG have all contributed to a decline in the frequency of CABG procedures that need to be redone.
Need
Patients may need to be considered for recurrent coronary artery bypass graft (CABG) surgery due to the grafts’ inevitable deterioration over time. After a second CABG, long-term survival is equivalent to PCI. Patients with viable LAD area should be the only ones for whom a redo CABG is indicated. The surgical outcomes of a redo CABG have also been improved by numerous technical advancements. The correct myocardial protection was substantially aided by retrograde cardioplegia, particularly when the blocked coronary arteries were fed with patent in situ arterial grafts. A certain, more comorbid population may benefit from the off-pump method, which has been employed in redo CABG.
Process
Techniques both on-pump and off-pump have been used successfully. The choice of on-pump or off-pump treatment depends on the required surgical access. Even while redo CABG surgeries frequently take substantially longer, a sizable portion of that time is spent doing the initial exposure and establishing the bypass circuit.
For initial exposure, the majority of surgeons use the same general strategy, which includes a median sternotomy. The prior incisional scar of a patient is frequently attempted to be retraced by surgeons. As a result of adhesions and scarring, they may also have to remove sternal wires, which can be challenging in some cases. Unlike a primary sternotomy, most surgeons won’t ask for the lungs to be deflated because they expect the dissection and exposure to take a lot longer.
Similar to first CABG, the aim of redo CABG is to achieve full revascularization. The use of various arterial grafting procedures during initial CABG may eliminate the requirement for a second CABG, significantly reducing the necessity for repeat CABG in the future. Nevertheless, should the necessity arise, redo CABG would be difficult since patients would almost certainly have additional comorbidities, more convoluted coronary anatomy, and left ventricular failure. Increased usage of less invasive techniques avoiding sternal re-entry and without the use of CPB would be advantageous for the future of redo CABG. The patient would benefit from “the best of both worlds” if hybrid revascularization was achieved by the combination of PCI and off-pump CABG.
Redo CABG is a complicated procedure, and the best results require careful planning and precise surgical technique. Both the off-pump and on-pump strategies may be beneficial to surgeons who do redo CABG surgeries in a variety of anatomical scenarios. It is becoming less common, which further increases the difficulty of doing this extremely difficult surgical treatment. The mortality rate of redo CABG has been lowered to be comparable to that of original CABG in surgical facilities with skilled surgeons.
About
The heart is a muscle-powered pump. It has two atria in the upper chambers and two ventricles in the lower chambers, totaling four pumping chambers. Blood flows forward through the heart thanks to valves located between each of its pumping chambers.
Need
It may be necessary to repair or replace valves if they are harmed, diseased, or otherwise not functioning properly. Valve stenosis (stiffness) and valve regurgitation are conditions that can result in heart valve malfunction (leaky valve).
The heart must work harder to pump blood through stenotic (stiff) valves, which can affect one or more valves. Aging, infections (such staph or rheumatic fever), and narrowing of the valves can cause these changes. Blood flows backwards if one or more valves are damaged, which reduces the amount of blood pumped in the proper direction. Your healthcare professional may determine that the defective valve(s) needs to be surgically repaired or replaced based on your symptoms and the state of your heart overall.
You may experience the following signs of heart valve disease or damage:
- chest pain
- breathing problems
- Palpitations
- Dizziness
- Swelling in your ankles, feet, or abdomen (belly)
- fluid retention-related rapid weight gain
Your doctor might advise heart valve replacement or repair surgery for additional causes.
Process
Heart valve replacement or repair has historically been done through open-heart surgery. This entails making a significant incision in the chest and temporarily stopping the heart so the surgeon may fix or replace the valve (s). To replace or repair heart valves, more recent, minimally invasive procedures have been developed. Smaller incisions, reduced postoperative pain, and shorter hospital stays are all benefits of minimally invasive surgeries.
The unhealthy valve may be replaced with an artificial valve or repaired using a ring to support the damaged valve. Tissue or carbon-coated plastic may be used to make artificial valves. The benefits and drawbacks of each type will be discussed, as well as which option may be ideal for you, with your healthcare physician.